Use of essential oil-containing mouthrinses by xerostomic individuals: determination of potential for oral mucosa irritation23
- Fischman SL, Aguirre A, Charles CH. Am J Dent. 2004;17(1):23-36.
Objective
Assess the irritation potential of an essential oil-containing mouthrinse (LISTERINE® Antiseptic) in a population with objectively documented xerostomia (hyposalivation) using an exaggerated-exposure clinical model (N=18).
Methodology
Observer-blinded crossover study of subjects (aged ≥18 years) with a history of xerostomia secondary to medication or Sjorgren’s syndrome and an unstimulated salivary flow rate of <0.25 mL/minute.
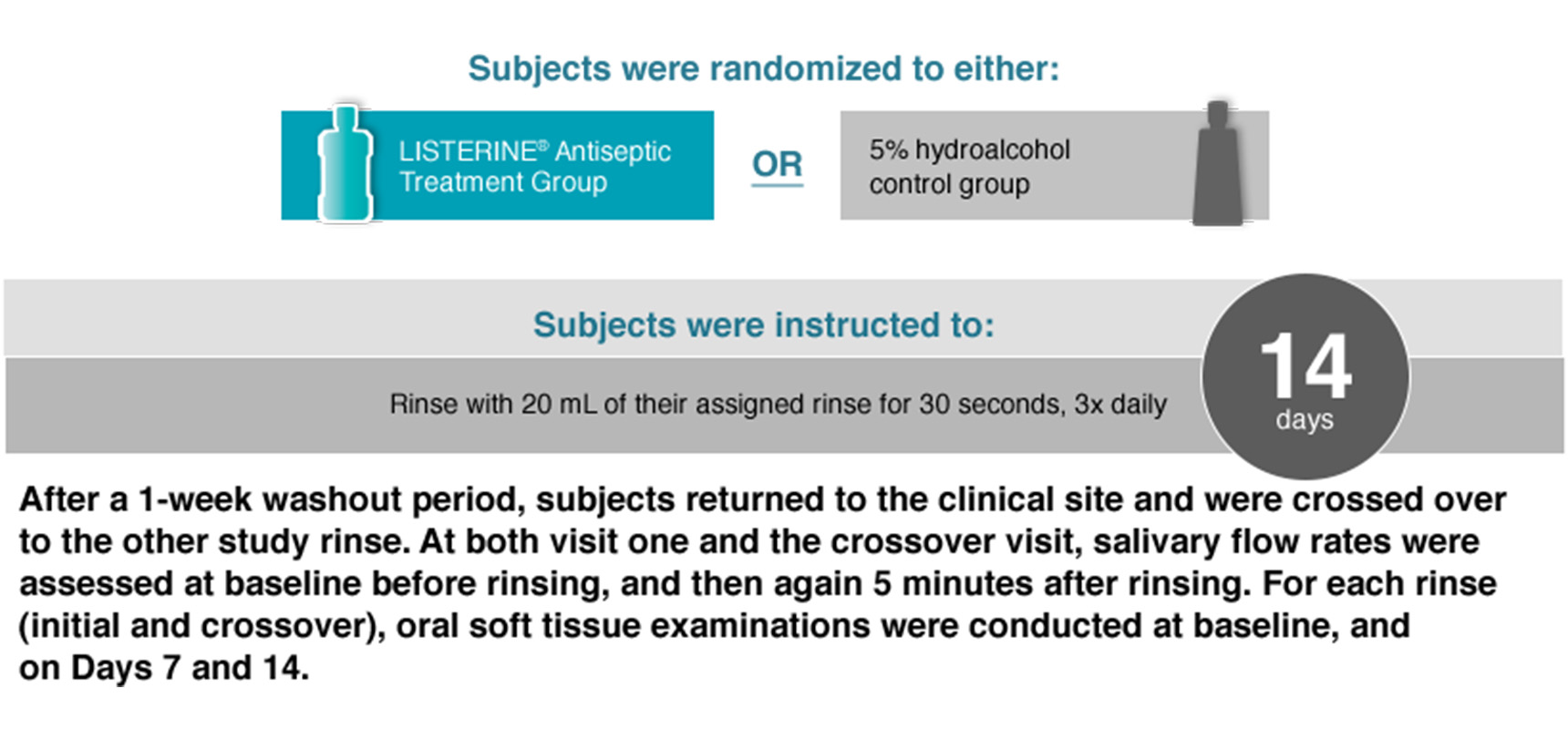
Subjects were randomized to either
LISTERINE® Antiseptic Treatment Group OR 5% hydroalcohol control group
Subjects were instructed to:
Rinse with 20 mL of their assigned rinse for 30 seconds, 3x daily 14 days
After a 1-week washout period, subjects returned to the clinical site and were crossed over to the other study rinse. At both visit one and the corssover visit, salivary flow rates were assessed at baseline before rinsing, and then again 5 minutes after rinsing. For each rinse (initial and crossover), oral soft tissue examinations were conducted at baseline, and on Days 7 and 14.
Results
The oral irritation potential of the essential oil mouthrinse was minimal.
- All subjects tolerated the mouthrinses well
- With the exception of 2 subjects, none developed oral mucosal lesions during the course of the study that could be attributable to the test rinses
- 2 subjects had an asymptomatic “whitish slough” of the buccal mucosae after rinsing with the essential oil mouthrinse for 7 days (wiped off readily, leaving a normal appearing, non-erythematous mucosa). In both subjects, the mucosae appeared normal at the 14-day exam.
Conclusion
LISTERINE® Antiseptic does not dry out tissues and may increase the salivary flow rate.
Exaggerated use of the essential oil mouthrinse did not result in any observed oral dryness compared to the control rinse or in a clinically significant difference in oral irritation, even in this xerostomic population that would be the most vulnerable to “drying.”
Safety & Tolerability
Find out more about LISTERINE® Brand products’ safety and tolerability.